CHOC
Children’s health information
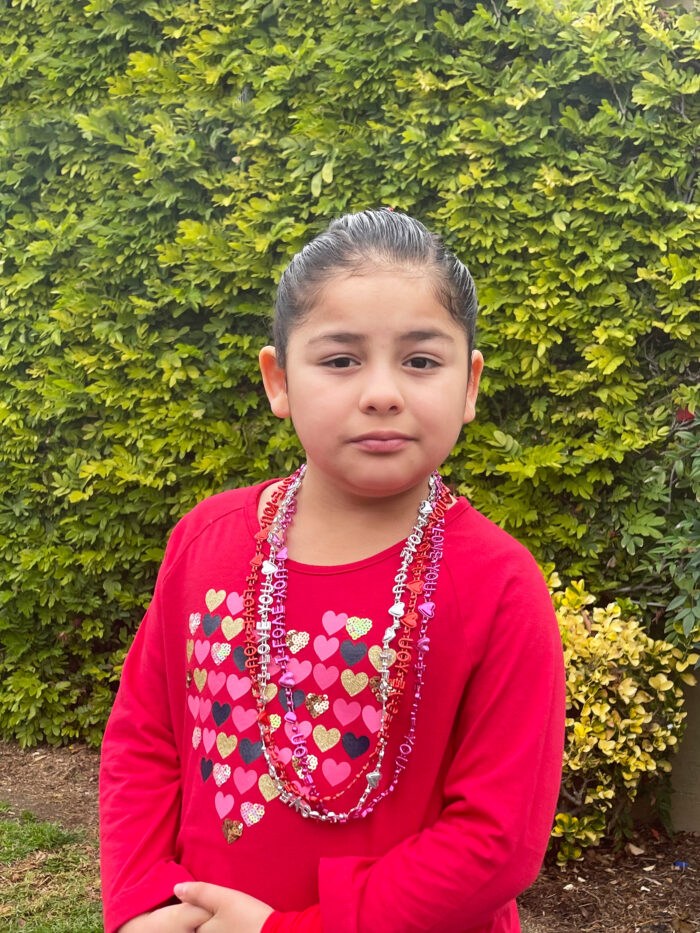
Celebrate differences
Search
Browse by topic
April is World Autism Month
At the Thompson Autism and Neurodevelopmental Center at CHOC, our goal is to help children reach their maximum potential — no matter what it looks like for them. Hear stories and get advice from CHOC experts.
Call CHOC’s free 24/7 Nurse Advice Line
Our free nurse helpline is open 24/7 to address questions about your child’s health.
Long Live Childhood Podcast
CHOC’s pediatric health and wellness podcast features pediatric experts who address top parenting concerns and provide tips to keep children happy and healthy.
DEVELOPMENT

Ages & Stages
KidsHealth Newsletter
Get the latest news, parenting tips and more health information from the pediatric experts at CHOC delivered straight to your inbox.