
ARTICLE

ARTICLE

ARTICLE

ARTICLE

ARTICLE

ARTICLE
ARTICLE

ARTICLE

ARTICLE

ARTICLE

ARTICLE
ARTICLE

ARTICLE

ARTICLE

ARTICLE

ARTICLE

ARTICLE
.

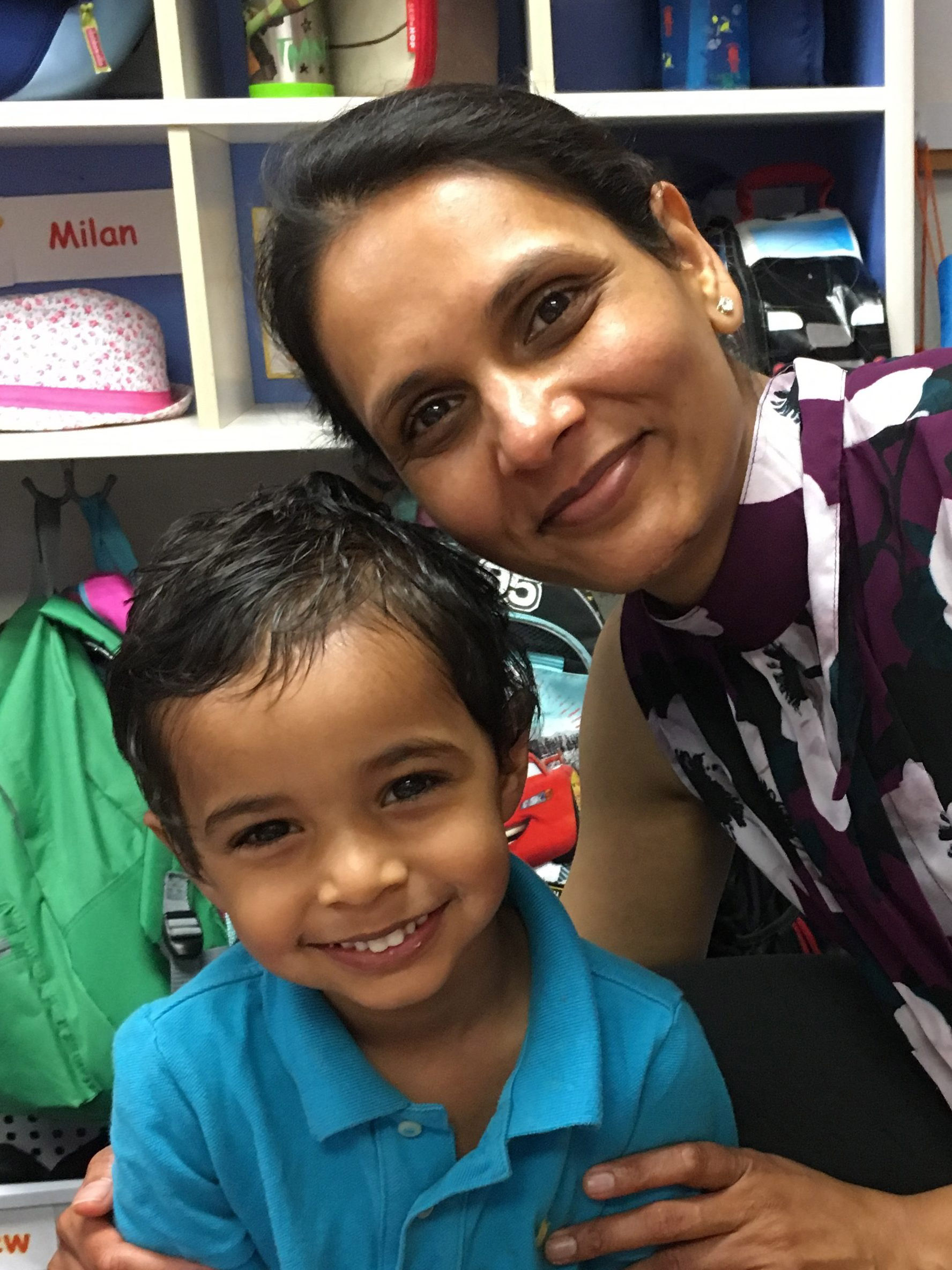
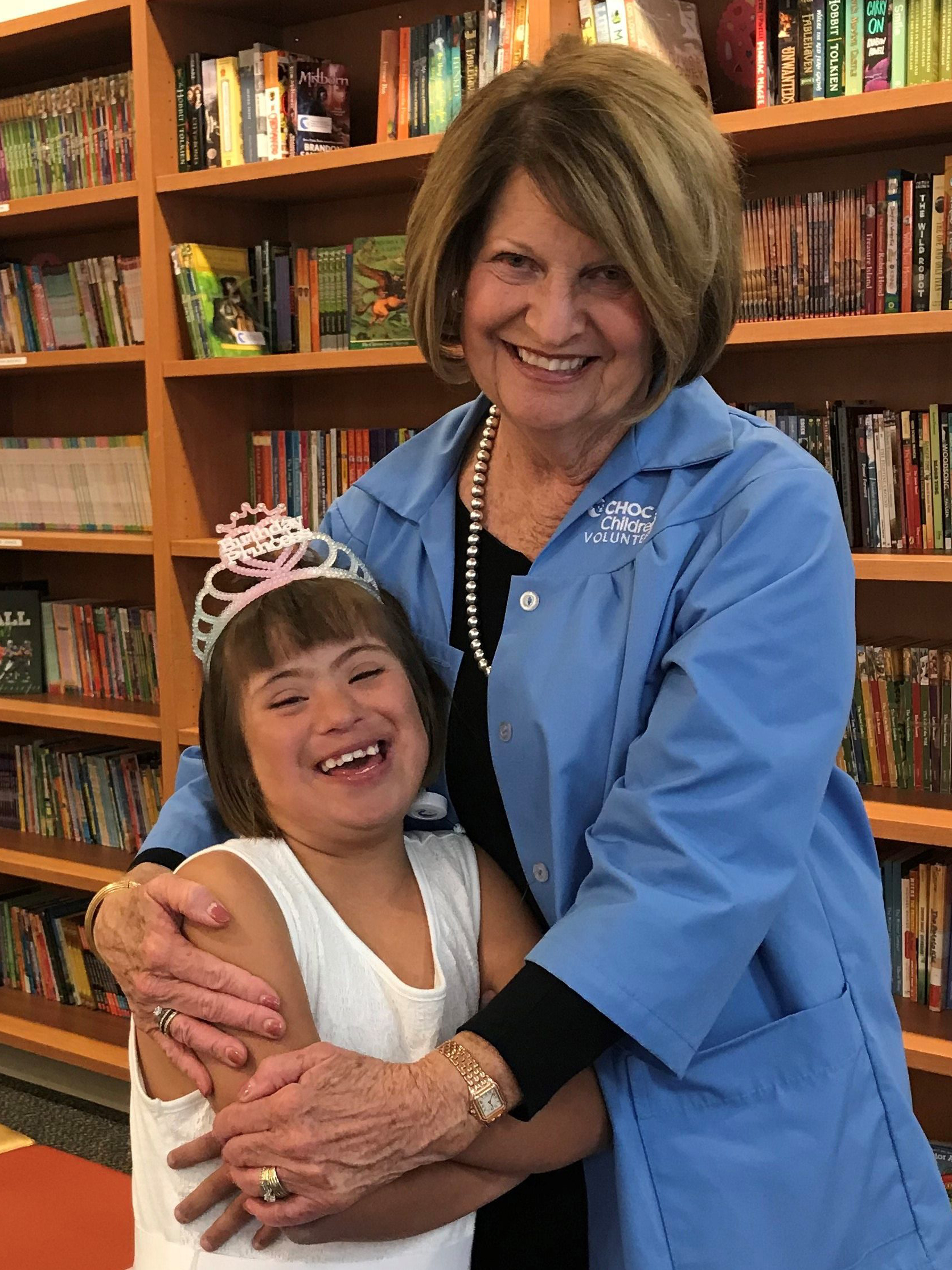
Our pediatric healthcare system is dedicated to preserving the magic of childhood.
